
PATIENT PORTAL
Pay My Bill
ALL ABOUT OUR SERVICES
Carpal Tunnel Surgery
Carpal tunnel is a safe and effective treatment
Cubital Tunnel Surgery
A pinched “funny bone” is no laughing matter!
De Quervain's Release
De Quervain’s is a painful tendon entrapment …
Plasma-rich Protein (PRP) Injections
Many patients suffer from tendon and joint …
Tendon Repair
Repair of the tendons that bend and straighten our …
Thumb Carpometacarpal Arthroplasty
The thumb carpometacarpal joint, or CMC joint, is
Trigger Finger/Thumb Surgery
Trigger finger or trigger thumb can be a painful
Ulnar Shortening Osteotomy
The radius and ulna are the two long bones in our …
Ultrasound
With ultrasound imaging available in the office,

The thumb carpometacarpal joint, or CMC joint, is a very common place for arthritis to occur, especially in women. Debilitating joint pain at the thumb can also be managed quite successfully with non-operative methods, such as bracing, exercise regimen, medications, and injections, but sometimes the pain persists and limits our quality of life. Fortunately there are surgical procedures to help treat those thumbs that cannot.
Treatment Options
Surgical treatment of arthritis at the carpometacarpal (CMC) joint, or base of the thumb, is called arthroplasty. There are many variations in how the procedure can be performed, including:
* Hematoma distraction arthroplasty
* Ligament reconstruction & tendon interposition
* Suspensionplasty with mini tight rope
* Implant arthroplasty
* Arthroscopic resection, or hemiresection and interposition, arthroplasty
The common thread with each procedure is removal of all or part of the trapezium, which is the small bone below the thumb metacarpal. By removing this bone and is osteophytes (bone spurs), the pain is alleviated from the arthritic condition. By removing the bone, important ligaments are rendered useless and instability of the thumb may occur. This is where the variations in treatment come from.
Studies have shown that there isn’t a measurable difference in success, complications, or failures of the different types of surgery for treatment of thumb arthritis. The most common technique Dr. Larson uses is a complete trapeziectomy with Suspensionplasty. With a suspensionplasty, the trapezium is removed, but instead of transferring a patient’s tendon to recreate the function of the lost ligaments, a medical device that has 2 small buttons connected by strong suture material is passed from the base of the thumb metacarpal to the index finger metacarpal. The two small buttons act as anchors on the far sides of the metacarpals, and the strong suture material that makes up the device is tensioned to provide thumb stability. While there is an extra incision on the back of the hand that is needed to place the implant, this takes away the need to make a separate forearm incision and the need to sacrifice a nearby tendon. A suspensionplasty generally allows for earlier motion and less pain.
TRIGGER FINGER/THUMB SURGERY
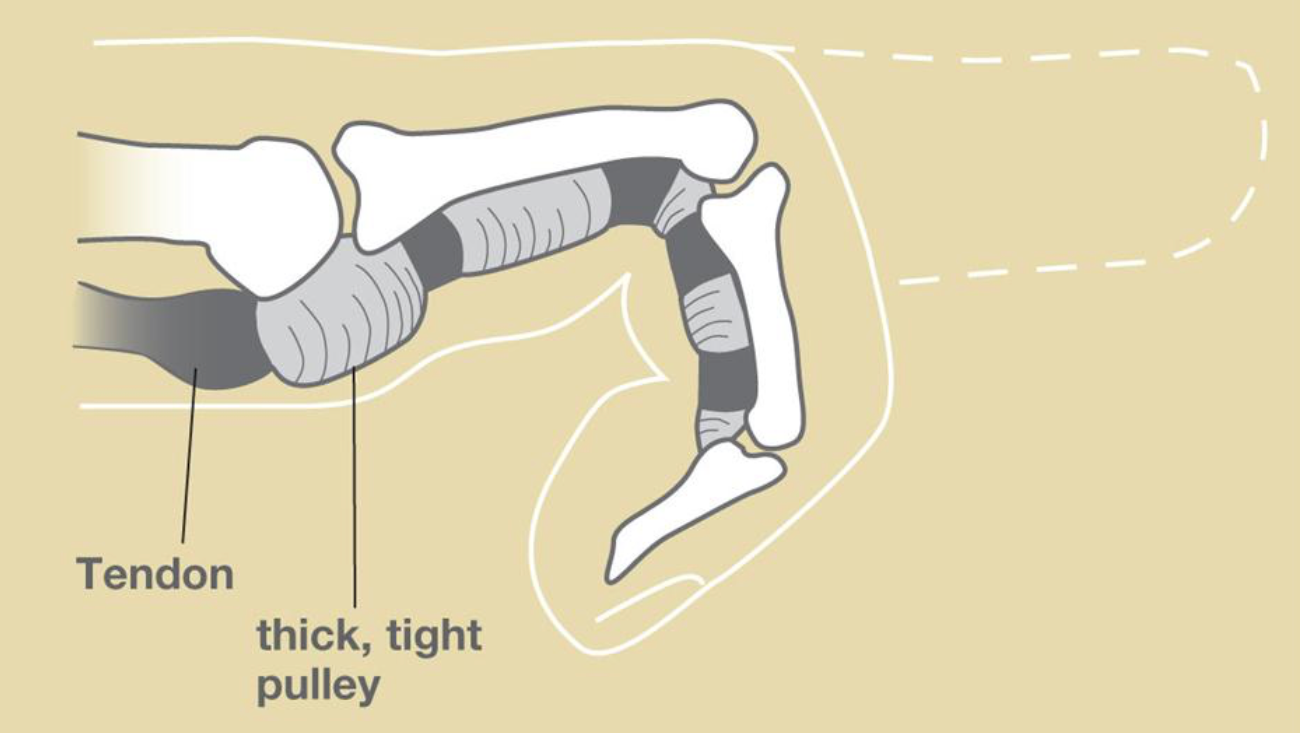
Trigger finger or trigger thumb can be a painful and aggravating condition. While it can often be cured with steroid injections, some fingers require a minor procedure to alleviate the pain and catching.
Trigger finger surgery is done under light sedation using intravenous medications such as propofol and a local anesthetic injection. A small, 1-1.5 cm incision is made in the end of the palm, just at the base of the finger, or in the flexion crease at the base of the thumb. The tendon sheath and tunnel system, or pulley, are identified, and a surgical knife is used to cut the start of the pulley system, alleviating the con stricture and triggering.
Once the release is done, the patient is allowed to awaken from the sedation and is asked to bend and straighten the finger to make sure no more catching or triggering occurs. Don’t worry – the finger has been numbed and there is no pain!! This confirms that the trigger finger has been appropriately taken care of. 2-3 sutures are then placed, and a small dressing is put over the incision.
The patient can remove the dressings 3 days after the procedure and use a small bandage to keep the wound covered. They are asked to move the fingers immediately after surgery and usually complete a short course of therapy.

The radius and ulna are the two long bones in our forearm that come together at the wrist to make a very unique, and sometimes finicky, wrist joint. We may develop problems if the ulna bone, the long bone of the forearm on the small finger side, is longer than the edge of the radius bone next to it. This may cause pain when we turn our wrist to the side.
Amongest other treatment options, shortening the ulna by a few millimeters can make a big difference in pain relief and improved function. The ulna can be shortened by a few different methods, but shortening of the ulnar shaft is the most common way. A saw is used to make a cut in the bone and the ends of the ulna are brought together firmly with a plate. The wrist will be protected in a splint for 2 weeks, and then in a removable splint for an additional 2-4 weeks.
If the small finger side of your wrist is causing pain or limiting your activities, please call the office.
CARPAL TUNNEL SURGERY

With ultrasound imaging available in the office, Dr. Larson is able to diagnose many conditions, including cysts, small masses, tendon disorders, and more. Ultrasound-guided needle placement provides for more accuracy and less pain when performing injections or aspirating cysts or joint effusion all over the body.
Ultrasound imaging can often save the need for more expensive and time-consuming MRI tests.

A pinched “funny bone” is no laughing matter! Sometimes the Ulnar Nerve (often referred to as the “funny bone’ as it runs behind your elbow) can become trapped or kinked if the elbow is hyper flexed during activities or sleep. Or, you may tend to lean or put pressure on the elbow such as when driving, keyboarding, or using an armrest or wheelchair.
Similar to Carpal Tunnel Syndrome, the symptoms of Cubital Tunnel Syndrome include numbness, tingling, and burning in the fingers, palm, and forearm. The symptoms tend to be more in the small and ring finger side of the hand, but often the symptoms are as subtle as an “odd sensation” in the palm. Nerve studies can be useful in making the diagnosis of Cubital Tunnel Syndrome, but can be falsely negative (meaning that the disease is present despite a negative test).
at the elbow can be indicated. Usually the nerve can be decompressed and left in its natural position, but it may need to be moved, or transposed, to a position in front of the elbow. Surgery is done an outpatient procedure, and a short course of therapy can help speed up your recovery. Splinting after surgery is only needed if the nerve needs to be transposed.
DE QUERVAIN'S RELEASE

De Quervain’s is a painful tendon entrapment condition that affects the thumb side of the wrist. Surgery can be performed to alleviate the compression and provide relief. This can be done under local anesthetic (with no sedation), or with moderate sedation or a general anesthetic. The steps to the release are simple, but delicate.
First, the arm is prepped and IV antibiotics are given to help prevent infection. Local anesthetic is then given, and a tourniquet placed just below the elbow is inflated. Next, the location of the tendons within the first dorsal compartment is located and an incision is made. There is a small sensory nerve branch that is predictably nearby. This nerve is located and protected while the underlying tendons are identified underneath a thick band of tissue covering them, called the retinaculum.
With precision, the retinaculum is then cut in line with the tendons, releasing the retinaculum and allowing the tendons to free themselves from compression. There may be thickening of the lining of the tendons, or thickening of the floor of the retinaculum. These thickened tissues can be trimmed or taken out if needed to allow the tendons to be free to glide and move smoothly.

Many patients suffer from tendon and joint disorders. An important aspect of treatment often includes restoring blood flow and allowing the body to more naturally heal itself. A key component of this is Platelet-Rich Plasma therapy, or PRP.
PRP therapy is an injection of a concentrated amount of a patient’s own platelets, which contain growth factors and inflammatory mediators that stimulate angiogenesis (new blood vessel formation) and healing of chronic conditions. This process is done in about 15-20 minutes, and involves drawing a small amount of blood from the patient, placing the sample in a centrifuge to separate the desired platelet concentration, and then performing a tendon or joint injection with the concentrated solution.
At Denton Hand and Orthopedics, we are pleased to offer this service as part of our comprehensive care for tendon and joint disorders.
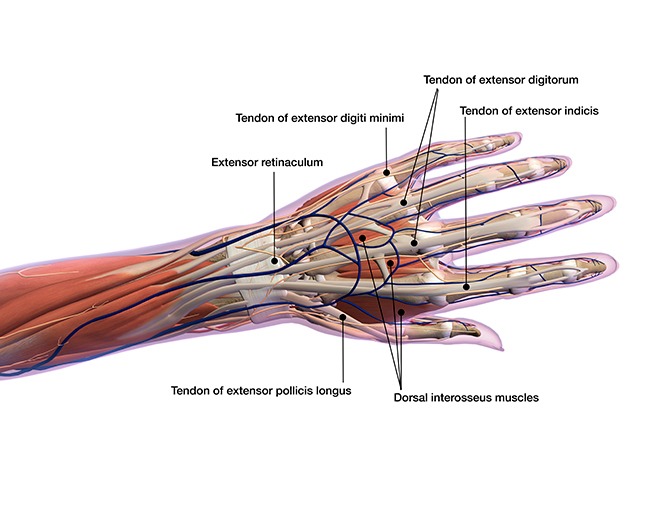
TENDON REPAIRTENDON REPAIR

Repair of the tendons that bend and straighten our fingers require specialty surgical training, and careful rehabilitation with the supervision of a certified hand therapist. Tendons that are repaired on the flexor, or palm side of the hand, require early motion with careful therapy guidance to avoid stiffness but allow time for the tendon to heal. Injuries to the nerves and blood vessels in the hand may occur at the same time and may also need repair and therapy.
On the contrary, tendons on the extensor, or backside of the fingers or hand, usually benefit from a short period of immobilization in a splint or cast before beginning motion and therap.
Tendonlaceration and injuries can be devastating injuries to the function of the hand. Surgery is most effective when done within 1-2 weeks of the injury, so please do not hesitate to call and schedule an appointment.

With ultrasound imaging available in the office, Dr. Larson is able to diagnose many conditions, including cysts, small masses, tendon disorders, and more. Ultrasound-guided needle placement provides for more accuracy and less pain when performing injections or aspirating cysts or joint effusion all over the body.
Ultrasound imaging can often save the need for more expensive and time-consuming MRI tests.
With nearly 20 years of ultrasound experience, Dr. Larson is pleased to offer this service in the office.
CALL THE OFFICE
BACK TO THE TOP
CONTACT US
Email checked during normal business hours.
