PATIENT PORTAL
Pay My Bill
SURGERY SERVICES
Carpal Tunnel
Cubital Tunnel Release
Finger Fracture (Phalanx & Metacarpal) Surgery
Wrist Fracture Surgery
Scaphoid Fracture and Non-Union Repair
Forearm And Elbow Fracture Surgery
Flexor and Extensor Tendon Repair
Wrist & Elbow Arthroscopy
Thumb Arthritis Surgery
Hand Small Joint Arthroplasty
Tendon Transfer
Hardware Removal
Cubital Tunnel Release
Finger Fracture (Phalanx & Metacarpal) Surgery
Wrist Fracture Surgery
Scaphoid Fracture and Non-Union Repair
Forearm And Elbow Fracture Surgery
Flexor and Extensor Tendon Repair
Wrist & Elbow Arthroscopy
Thumb Arthritis Surgery
Hand Small Joint Arthroplasty
Tendon Transfer
Hardware Removal
There are two techniques for performing carpal tunnel surgery: open or endoscopic. Open surgery involves a 1.5-2 inch incision at the base of the palm, and allows the surgeon to dissect down to the transverse carpal ligament (the structure pinching the nerve). The surgeon then releases the ligament, as well as any fascia, or connective tissue, in the palm or forearm that may be compressing the nerve.
The other option is to use an endoscope, which allows the ligament to be divided from within the carpal tunnel itself, avoiding the skin and muscle dissection in the palm. The endoscope, which is placed at one end of a thin, cylinder tube is inserted into the carpal tunnel by making a small (< 1-inch) incision at the wrist. At the other end of the tube, there is a sharp blade that can be raised to cut the ligament.
Studies have suggested that endoscopic carpal tunnel release has less pain and time missed from work, while being equally as safe and effective. Dr. Larson routinely performs both open and endoscopic carpal tunnel release. Each patient is unique, and some Based upon each specific patient’s condition, wrist history, and use of the hand, an individualized surgical treatment plan is selected together
The other option is to use an endoscope, which allows the ligament to be divided from within the carpal tunnel itself, avoiding the skin and muscle dissection in the palm. The endoscope, which is placed at one end of a thin, cylinder tube is inserted into the carpal tunnel by making a small (< 1-inch) incision at the wrist. At the other end of the tube, there is a sharp blade that can be raised to cut the ligament.
Studies have suggested that endoscopic carpal tunnel release has less pain and time missed from work, while being equally as safe and effective. Dr. Larson routinely performs both open and endoscopic carpal tunnel release. Each patient is unique, and some Based upon each specific patient’s condition, wrist history, and use of the hand, an individualized surgical treatment plan is selected together
Carpal tunnel is a safe and effective treatment option for patients who have persistent pain and dysfunction of their hand due to carpal syndrome that does not respond to splinting, therapy, or injections. Surgery is done under either a local or general anesthetic, and is a routing, outpatient procedure. The goal of the surgery is to release the transverse carpal ligament (the structure pinching the nerve), thereby allowing for more room within the carpal tunnel and thus less pressure on the nerve.
A pinched “funny bone” is no laughing matter! Sometimes the Ulnar Nerve (often referred to as the “funny bone’ as it runs behind your elbow) can become trapped or kinked if the elbow is hyper flexed during activities or sleep. Or, you may tend to lean or put pressure on the elbow such as when driving, keyboarding, or using an armrest or wheelchair.
Similar to Carpal Tunnel Syndrome, the symptoms of Cubital Tunnel Syndrome include numbness, tingling, and burning in the fingers, palm, and forearm. The symptoms tend to be more in the small and ring finger side of the hand, but often the symptoms are as subtle as an “odd sensation” in the palm.
When non-operative treatment fails, release of the ulnar nerve at the elbow can be indicated. Usually the nerve can be decompressed and left in its natural position, but it may need to be moved, or transposed, to a position in front of the elbow. Surgery is done an outpatient procedure, and a short course of therapy can help speed up your recovery.
Similar to Carpal Tunnel Syndrome, the symptoms of Cubital Tunnel Syndrome include numbness, tingling, and burning in the fingers, palm, and forearm. The symptoms tend to be more in the small and ring finger side of the hand, but often the symptoms are as subtle as an “odd sensation” in the palm.
When non-operative treatment fails, release of the ulnar nerve at the elbow can be indicated. Usually the nerve can be decompressed and left in its natural position, but it may need to be moved, or transposed, to a position in front of the elbow. Surgery is done an outpatient procedure, and a short course of therapy can help speed up your recovery.
Finger fractures, involving the phalanx or metacarpal bones, can significantly affect hand function and overall quality of life. In cases where the fracture is displaced or unstable, surgical intervention may be necessary to restore proper alignment and promote optimal healing.
Finger fracture surgery involves repositioning the broken bones and securing them with screws, plates, or wires. This procedure aims to realign the bones accurately, enabling the fingers to regain their normal shape and function. Following the procedure, patients are often advised to undergo rehabilitation therapy to restore hand strength and range of motion.
Therefore, it is crucial to consult with a qualified orthopedic surgeon, who can assess the severity of the fracture and determine the most appropriate treatment option. Prompt surgical intervention for finger fractures can lead to a faster recovery and improved hand functionality, allowing patients to regain their normal activities in the shortest possible time.
Finger fracture surgery involves repositioning the broken bones and securing them with screws, plates, or wires. This procedure aims to realign the bones accurately, enabling the fingers to regain their normal shape and function. Following the procedure, patients are often advised to undergo rehabilitation therapy to restore hand strength and range of motion.
Therefore, it is crucial to consult with a qualified orthopedic surgeon, who can assess the severity of the fracture and determine the most appropriate treatment option. Prompt surgical intervention for finger fractures can lead to a faster recovery and improved hand functionality, allowing patients to regain their normal activities in the shortest possible time.
The hand and wrist are very unique and high-functioning parts of our body. Broken bones, or fractures, can cause a lot of disruption to our lives, even if only minimal treatment is required. Some fractures, such as a wrist fracture that occurred from a simple fall onto an outstretched hand, can indicate weakening of the skeleton or osteoporosis.
Surgery may be indicated when the fracture is displaced, or shifted, or involve nearby joints.
Often, surgery can help expedite recovery, and allow less dependence on casts or splints, helping us regain function and perform all of the wonderful activities that our hands let us do. Some fractures require percutaneous fixation and insertion of wires, while other surgeries require incisions and direct fixation of the bone. Some injuries may have happened in the past and may require bone grafting and more technical procedures. Dr. Timothy Larson, an orthopedic surgeon with fellowship-developed skill in hand and upper extremity procedures, is well trained to help your hand and wrist fracture.
Surgery may be indicated when the fracture is displaced, or shifted, or involve nearby joints.
Often, surgery can help expedite recovery, and allow less dependence on casts or splints, helping us regain function and perform all of the wonderful activities that our hands let us do. Some fractures require percutaneous fixation and insertion of wires, while other surgeries require incisions and direct fixation of the bone. Some injuries may have happened in the past and may require bone grafting and more technical procedures. Dr. Timothy Larson, an orthopedic surgeon with fellowship-developed skill in hand and upper extremity procedures, is well trained to help your hand and wrist fracture.
A scaphoid fracture is a common injury that occurs in the wrist, specifically in the scaphoid bone. This small bone is situated at the base of the thumb and is crucial for proper hand function. A scaphoid fracture often happens due to falls or impacts, causing immense pain and swelling in the wrist. If left untreated, this injury can lead to non-union, which means that the bone does not heal properly. Non-union occurs when the bone fails to reunite, and the lack of blood supply to the fractured area hinders the natural healing process.
To repair a scaphoid non-union, medical intervention is necessary. A surgical procedure called a bone graft may be performed, where bone tissue is taken from another area of the body or a donor and placed over the fracture site to stimulate new bone growth. In some cases, metal screws or pins may be used to stabilize the bone during the healing process. With prompt treatment and appropriate medical care, scaphoid fractures and non-unions can be effectively repaired, allowing individuals to regain their hand function and resume their daily activities.
To repair a scaphoid non-union, medical intervention is necessary. A surgical procedure called a bone graft may be performed, where bone tissue is taken from another area of the body or a donor and placed over the fracture site to stimulate new bone growth. In some cases, metal screws or pins may be used to stabilize the bone during the healing process. With prompt treatment and appropriate medical care, scaphoid fractures and non-unions can be effectively repaired, allowing individuals to regain their hand function and resume their daily activities.
Forearm and elbow fractures are common injuries that often require surgery for proper treatment and healing. These fractures occur as a result of falls, sports injuries, or direct blows to the arm. Surgery is typically recommended when the bone fragments are displaced or if there is an open fracture. The main goal of forearm and elbow fracture surgery is to realign the broken bones and stabilize them to enable proper healing.
The surgery is usually performed under general anesthesia, and the surgeon may use screws, plates, or rods to hold the bones in place. Once the bones are properly aligned and fixed, the surgeon will close the incision with sutures. Following the surgery, patients will typically need to undergo a period of immobilization, such as wearing a cast or splint. Physical therapy is also an important component of the recovery process to help restore strength, flexibility, and function to the forearm and elbow. With appropriate surgery and rehabilitation, most patients can regain full range of motion and return to their normal activities.
The surgery is usually performed under general anesthesia, and the surgeon may use screws, plates, or rods to hold the bones in place. Once the bones are properly aligned and fixed, the surgeon will close the incision with sutures. Following the surgery, patients will typically need to undergo a period of immobilization, such as wearing a cast or splint. Physical therapy is also an important component of the recovery process to help restore strength, flexibility, and function to the forearm and elbow. With appropriate surgery and rehabilitation, most patients can regain full range of motion and return to their normal activities.
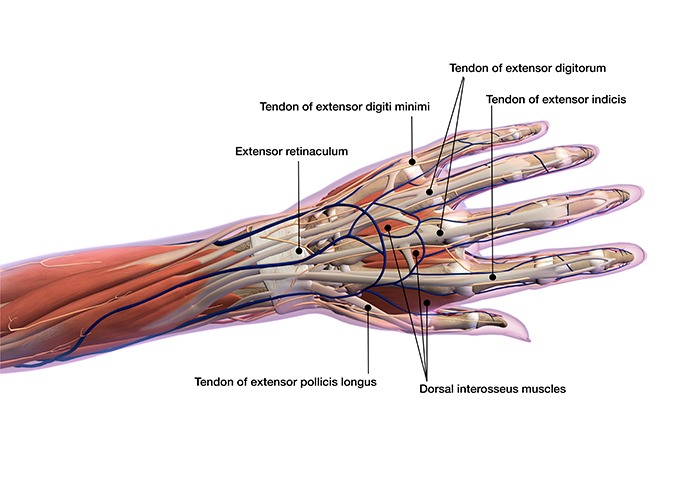
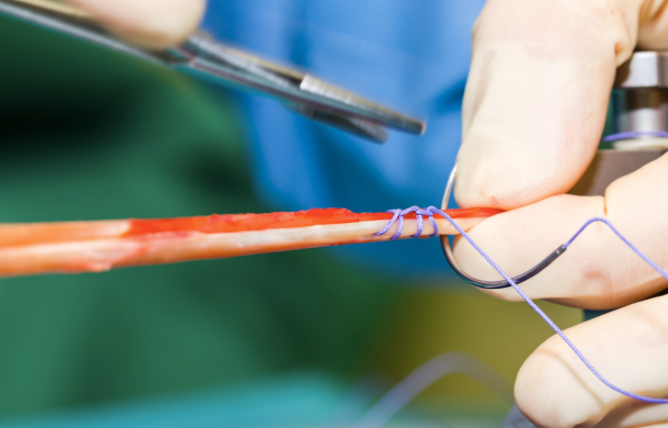
Flexor and extensor tendon repair is a surgical procedure commonly performed to restore the normal function of damaged tendons in the hand, wrist, and fingers. Flexor tendons are responsible for flexing or bending the fingers, while extensor tendons are responsible for extending or straightening them. These tendons are vital for the normal range of motion and dexterity of the hand. Tendon injuries can occur due to trauma, such as cuts or lacerations, or from overuse or repetitive stress.
The repair procedure involves meticulously reattaching the severed or damaged tendon ends, usually with the help of sutures or small metal implants, to ensure proper alignment and healing. Following surgery, patients undergo a period of immobilization and rehabilitation, which may include splinting, hand therapy, and controlled movement exercises. The success of tendon repair depends on various factors, including the location and severity of the injury, the patients age and overall health, and the expertise of the surgical team. Early intervention and adherence to post-operative care instructions are crucial for achieving optimal outcomes and restoring full hand function.
The repair procedure involves meticulously reattaching the severed or damaged tendon ends, usually with the help of sutures or small metal implants, to ensure proper alignment and healing. Following surgery, patients undergo a period of immobilization and rehabilitation, which may include splinting, hand therapy, and controlled movement exercises. The success of tendon repair depends on various factors, including the location and severity of the injury, the patients age and overall health, and the expertise of the surgical team. Early intervention and adherence to post-operative care instructions are crucial for achieving optimal outcomes and restoring full hand function.
Wrist and elbow arthroscopy is a minimally invasive surgical procedure used to diagnose and treat various conditions affecting these joints. Arthroscopy involves the insertion of a small camera, called an arthroscope, into the joint through a small incision. This allows the surgeon to visualize and examine the structures inside the joint, such as bones, ligaments, tendons, and cartilage. The images captured by the camera are displayed on a monitor, providing a clear view of the joint and any abnormalities present.
The advantages of wrist and elbow arthroscopy include smaller incisions, reduced scarring, less pain, and faster recovery times compared to traditional open surgery.
This procedure can be used to manage a range of conditions, including ligament tears, tendonitis, bone spurs, arthritis, and loose bodies within the joint. Depending on the diagnosis, the surgeon may also perform additional procedures during arthroscopy, such as repairing or removing damaged tissue, smoothing out rough surfaces, or reattaching torn ligaments or tendons. Overall, wrist and elbow arthroscopy is a valuable surgical technique that provides patients with a less invasive treatment option and shortening their recovery time associated with traditional surgery.
The advantages of wrist and elbow arthroscopy include smaller incisions, reduced scarring, less pain, and faster recovery times compared to traditional open surgery.
This procedure can be used to manage a range of conditions, including ligament tears, tendonitis, bone spurs, arthritis, and loose bodies within the joint. Depending on the diagnosis, the surgeon may also perform additional procedures during arthroscopy, such as repairing or removing damaged tissue, smoothing out rough surfaces, or reattaching torn ligaments or tendons. Overall, wrist and elbow arthroscopy is a valuable surgical technique that provides patients with a less invasive treatment option and shortening their recovery time associated with traditional surgery.
The thumb carpometacarpal joint, or CMC joint, is a very common place for arthritis to occur, especially in women. Debilitating joint pain at the thumb can also be managed quite successfully with non-operative methods (steroid injections, PRP injection, braces, medicines, and therapy), but fortunately there are surgical procedures to help treat those thumbs that cannot.
Dr. Larson performs surgery for CMC arthritis of the thumb using one of several techniques, depending upon which one is the best for you. Arthroscopic debridement can be an option for early arthritis, as can thumb joint denervation - a procedure which removes the small nerve endings to the joint itself.
Most commonly, thumb arthritis surgery is performed by removing a small bone at the base of the thumb, the trapezium, and then using either the patient’s own tendon or a medical device to support the thumb. All of these procedures are excellent at treating pain and restoring thumb function.
Dr. Larson performs surgery for CMC arthritis of the thumb using one of several techniques, depending upon which one is the best for you. Arthroscopic debridement can be an option for early arthritis, as can thumb joint denervation - a procedure which removes the small nerve endings to the joint itself.
Most commonly, thumb arthritis surgery is performed by removing a small bone at the base of the thumb, the trapezium, and then using either the patient’s own tendon or a medical device to support the thumb. All of these procedures are excellent at treating pain and restoring thumb function.
Hand small joint arthroplasty is a surgical procedure performed to treat severe arthritis in the small joints of the hand, specifically the fingers and thumb. Arthritis in these joints can cause pain, stiffness, and limited range of motion, greatly affecting the hands functionality. During the procedure, the damaged joint surfaces are removed and replaced with artificial components, typically made of metal or plastic, to restore joint function and alleviate pain.
The surgery may be performed on one or multiple joints, depending on the severity of the arthritis and the patients needs. Hand small joint arthroplasty is considered a highly specialized procedure that requires a skilled orthopedic surgeon familiar with the complexities of the hand anatomy.
After the surgery, patients may go through a period of rehabilitation, which includes exercises to regain strength, flexibility, and functionality. Although hand small joint arthroplasty can greatly improve the quality of life for individuals with severe hand arthritis, it is important to carefully weigh the risks and benefits of the procedure with the surgeon before deciding to undergo surgery.
The surgery may be performed on one or multiple joints, depending on the severity of the arthritis and the patients needs. Hand small joint arthroplasty is considered a highly specialized procedure that requires a skilled orthopedic surgeon familiar with the complexities of the hand anatomy.
After the surgery, patients may go through a period of rehabilitation, which includes exercises to regain strength, flexibility, and functionality. Although hand small joint arthroplasty can greatly improve the quality of life for individuals with severe hand arthritis, it is important to carefully weigh the risks and benefits of the procedure with the surgeon before deciding to undergo surgery.
Tendon transfer is a surgical procedure that involves moving a tendon from one part of the body to another to restore or improve muscle function. This procedure is commonly performed to address conditions such as tendon rupture, muscle weakness, or loss of muscle function due to injury or disease.
During the surgery, a healthy tendon is detached from its original attachment site and reattached to a new location, allowing it to restore or augment muscle function. Tendon transfers can be utilized in various regions of the body, including the hand, foot, shoulder, and knee, depending on the specific needs of the patient. The surgery aims to enhance muscle strength, stability, and range of motion, ultimately improving overall function and quality of life.
Tendon transfers require careful planning and consideration, as they involve an intricate understanding of anatomy, biomechanics, and patient-specific requirements. While the procedure can be complex, it offers potentially significant benefits for individuals seeking to regain or enhance muscle function in areas affected by injury or disease.
During the surgery, a healthy tendon is detached from its original attachment site and reattached to a new location, allowing it to restore or augment muscle function. Tendon transfers can be utilized in various regions of the body, including the hand, foot, shoulder, and knee, depending on the specific needs of the patient. The surgery aims to enhance muscle strength, stability, and range of motion, ultimately improving overall function and quality of life.
Tendon transfers require careful planning and consideration, as they involve an intricate understanding of anatomy, biomechanics, and patient-specific requirements. While the procedure can be complex, it offers potentially significant benefits for individuals seeking to regain or enhance muscle function in areas affected by injury or disease.
Hand hardware removal is a medical procedure that involves the surgical extraction of metallic implants or foreign objects from the body. These implants can include screws, plates, wires, pins, or other devices that were previously inserted to aid in the healing process after a surgery or injury. The need for hardware removal may arise due to various reasons, such as pain, discomfort, infection, hardware failure, or the completion of the healing process.
The procedure is typically performed by a skilled orthopedic surgeon or medical professional in a sterile operating room. Prior to the removal, the area around the implant is cleaned and numbed with local anesthesia. A small incision is made near the implant, and the hardware is carefully detached and extracted from the body. Following the procedure, the incision is sutured, and a bandage is applied to promote proper healing.
Recovery time varies depending on the individual and specific circumstances, but most patients experience relief from the initial symptoms that prompted the hardware removal. Overall, hardware removal is a crucial procedure that aims to improve a patients quality of life and restore their mobility and comfort.
The procedure is typically performed by a skilled orthopedic surgeon or medical professional in a sterile operating room. Prior to the removal, the area around the implant is cleaned and numbed with local anesthesia. A small incision is made near the implant, and the hardware is carefully detached and extracted from the body. Following the procedure, the incision is sutured, and a bandage is applied to promote proper healing.
Recovery time varies depending on the individual and specific circumstances, but most patients experience relief from the initial symptoms that prompted the hardware removal. Overall, hardware removal is a crucial procedure that aims to improve a patients quality of life and restore their mobility and comfort.
CALL THE OFFICE
BACK TO THE TOP
CONTACT US
Email checked during normal business hours.